Get Quality Care TODAY At No Cost To You Or Your Family
We provide quality care to all who are in need, regardless of ability to pay.
- Medicare Part A
- AHCCCS
- Private Insurance
- No Insurance Or Coverage (Yep, we've got you covered)
OR...

Healthcare Professionals

You can refer patients and families to Soulistic Hospice with confidence that our highly qualified, diverse, and compassionate staff will provide expert, loving hospice care you want for your patients.
Your patients and their families are more likely to agree to hospice services when they have a conversation with you about it. At the time you determine that a cure is not possible and you make a referral to us, we’ll provide comfort with an emphasis on the quality of life of the patient, along with spiritual support for the family.
Soulistic Hospice admits patients every day, at any time, including evenings and weekends.
Referrals can be directly from you or the hospital. The referral can also be made after a patient is discharged to home or a facility.
We can meet with the patient and their family on the same day as the referral.
Payment Options
We accept hospice-eligible patients with Medicare, AHCCCS (Medicaid), and private insurance, as well as those without a primary caregiver. Call us about patients with financial hardship. We strive to serve everyone, regardless of ability to pay.
Hospice Eligibility
Hospice eligibility can vary, depending on many individual factors and co-morbidities.
If you have any questions about whether one of your patients qualifies for hospice care, please do not hesitate to call and speak to our Medical Director at (520) 398-2333.
Spiritual & Emotional Support
As a medical professional, you know when a cure is not possible. Since hospice emphasizes comfort and quality of life once an illness is incurable, it can improve the patient’s quality of life and extend the patient’s life. Yet many patients and families are reluctant to use hospice. When you have a conversation with them, they’re more likely to accept hospice services.
End-of-Life-Planning
During the difficult last stages of a serious illness, many people feel that they have lost control over their lives and what will happen to them. They don't realize that they regain control over their treatment by choosing hospice care. All too often, people delay asking their doctor about hospice services but when they finally do, they regret waiting so long. They learn that our patients and their family members are given the opportunity to make decisions that are important to them.
Veteran Support
We Honor Veteran partners who are on a mission to serve those who have served us. Soulistic Hospice has worked to build strong relationships with the Southern Arizona Veterans Association.
Medicare certified
Soulistic is locally owned and operated, faith-based, state licensed, Medicare certified. Our hospice care is fully covered under Medicare, Medicaid, and private insurance policies. We have worked hard to build strong relationships with the VA. As a nonprofit, we provide care regardless of a patient’s ability to pay.
Make a referral
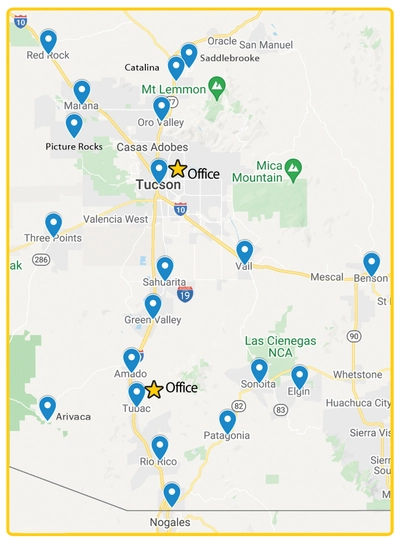
We provide expert, loving hospice care in Tucson, Oro Valley, Marana, Catalina, Saddlebrook, Red Rock, Picture Rocks, Three Points, Vail, Sahuarita, Green Valley, Arivaca, Amado, Tubac, Rio Rico, Nogales, Patagonia, Sonoita, and Elgin.
Fax (520) 398-9524

Facility Partners
Soulistic Hospice serves hospice patients in assisted living homes, skilled nursing facilities, and residential care facilities. Our collaboration with facility staff ensures seamless support for all the services we provide, including hospice care, palliative care consultation, pediatric care, and grief counseling.

Discharge Planners
Through direct referral from the hospital, or after a patient is discharged to home or a facility, Soulistic Hospice admits patients every day, at any time, including evenings and weekends. We can meet with the patient and their family on the same day as the referral. We accept hospice-eligible patients with Medicare, AHCCCS (Medicaid), and private insurance, as well as those without a primary caregiver. Call us about patients with financial hardship. We strive to serve everyone regardless of ability to pay.

Making the Referral
Soulistic Hospice is a nonprofit hospice specializing in providing the highest quality of end of life care. We are locally owned and operated, faith-based, state licensed, Medicare certified, and also VA contracted.

Diagnostic Guidelines
Hospice eligibility can vary depending on many individual factors and co-morbidities. Please do not hesitate to call and speak to our Medical Director at (520) 398-2333 if you have any questions about whether one of your patients would qualify for hospice care.

Having the Conversation
As a medical professonal, you cannot predict how soon your patient will transition, but you do know when a cure is not possible. Hospice emphasizes comfort and quality of life once an illness is incurable. Patients and families who are reluctant to use hospice are more likely to accept services when they have a conversation with their doctors about hospice care.
Read what families are saying about our expert, loving hospice care
Amazing
Over the past 5 years I have had three of my loved ones cared for by Soulistic Hospice during their passing. I am so very grateful to all of their caring staff for the quick responses to our needs
..."Read MoreAmazing
Over the past 5 years I have had three of my loved ones cared for by Soulistic Hospice during their passing. I am so very grateful to all of their caring staff for the quick responses to our needs any time day or night. My loved ones were always kept comfortable, and had their dignity maintained at all times. As the caregiver, I was given education on how to use medications when needed, and how to use the medical equipment they provided. This was so helpful. With the loss of my loved ones, Soulistic has provided me with bereavement support for as long as I need. It has been so wonderful to never feel alone. I would highly recommend Soulistic’s service to anyone needing hospice care.Hana
We Can't Thank Soulistic Hospice Enough
I can't thank Soulistic Hospice enough for the all-around comfort, care and support you gave us, nurturing our body, mind, spirit, and heart. Together, on this part of our journey, we got the most
..."Read MoreWe Can't Thank Soulistic Hospice Enough
I can't thank Soulistic Hospice enough for the all-around comfort, care and support you gave us, nurturing our body, mind, spirit, and heart. Together, on this part of our journey, we got the most out of life.Sue and Joe
I don't know how I would have made it through without them.
My husband was with Soulistic Hospice, in their palliative care program for over 2 years. Both of us were constantly amazed at the care and concern given to both of us. I don't know how I would have
..."Read MoreI don't know how I would have made it through without them.
My husband was with Soulistic Hospice, in their palliative care program for over 2 years. Both of us were constantly amazed at the care and concern given to both of us. I don't know how I would have made it through those care giving years without them, as I had very painful issues of my own. Whatever equipment or supplies he needed, they provided. The spiritual staff was always available to me either by phone or in person. Each week, he looked forward to his 3 showers, as she was so kind, gentle and sang to him...sometimes Spanish, sometimes English; he didn't care. Twice, he had to go off their weekly care due to emergency hospital stays; but as soon as he was released, they were at the house on the same day, to get him back into the program. The nurses were incredible in keeping a close monitor on him, and me as well; and even followed him to an assisted living home. His nurse went above and beyond in trying to get the home staff to administer his meds correctly. I truly can't imagine getting any better assistance from anyone than with Soulistic Hospice.L. Durocher
So very happy.
Eileen
Above & Beyond
I have referred to Soulistic Hospice on a number of occasions. They are by far the most compassionate and organized hospice company I have encountered. They are quick and responsive when contacted
..."Read MoreAbove & Beyond
I have referred to Soulistic Hospice on a number of occasions. They are by far the most compassionate and organized hospice company I have encountered. They are quick and responsive when contacted and are always available same day, sometimes same hour. Their liaison, goes above and beyond to make sure our patients and their families are well taken care of from start to finish. If I could give them a 10 star I would!Shelly R.
Skilled Nursing, Tucson
Outstanding
Soulistic Hospice took such fantastic care of my husband during his last days. The care and compassion that everyone at Soulistic showed to us during this tough time was outstanding. The entire team
..."Read MoreOutstanding
Soulistic Hospice took such fantastic care of my husband during his last days. The care and compassion that everyone at Soulistic showed to us during this tough time was outstanding. The entire team was so helpful and knowledgeable about the situation and the uncertainties the patients and families are going through. There was someone available 24/7 if there was a question or problem. The nurses were so kind and caring; they explained everything to me, what they were doing and what my husband was going through. The CNAs that came out to help were incredibly gentle and respectful. I am truly grateful for them. They made my husband's last days easier.Marcia P.
We highly recommend them
We highly recommend them
I cannot recommend this hospice enough. We searched through every hospice in Tucson to try and find the right one for my mom, and we are so thankful that we chose this one. I had no idea what hospice was about, but I don't know how we would have gotten through my mom's last months without them. We highly recommend them.Selena M.
I highly recommend this company.
This year I had the direct experience of receiving hospice care for a loved one that I was caring for in my home. I have had experiences with two other hospices in the area. Soulistic was there to
..."Read MoreI highly recommend this company.
This year I had the direct experience of receiving hospice care for a loved one that I was caring for in my home. I have had experiences with two other hospices in the area. Soulistic was there to help immediately and provided thorough service from medications and equipment to appropriate emotional support at a time when all those things were so needed. There were a few months before my loved one passed when the Soulistic team came to visit regularly while there was time to talk and listen to my dear friend. The nurses monitored his symptoms and adjusted things as he came closer to his end of life. They would check in with me also and made sure we both knew what to expect. It was a blessing to have Soulistic services during our time of need. They helped both me and my loved one, and it was so helpful to know that they were there to call on at any time. I highly recommend this company for their ability to help people at a difficult time with heart and professionalism.Cbonzani
One of the Finest
One of the Finest
Soulistic hospice is one the finest organizations we have ever encountered. As a group dedicated to caring for the terminally ill, or people in severe distress, they have been totally dedicated to our service. The staff is always courteous and helpful, going out of their way to aid people in their care.David
Excellent care
Excellent care. Very compassionate. Could not have asked for more.They were so attentive and comforting to the client and care giver. I highly recommend them and so grateful for their
..."Read MoreExcellent care
Excellent care. Very compassionate. Could not have asked for more.They were so attentive and comforting to the client and care giver. I highly recommend them and so grateful for their care!Mariela M.
The staff at Soulistic were incredible.
The staff at Soulistic were incredible. Bonnie, Camille, Debbie and Jennifer went above and beyondto make sure my mom was comfortable. Their team aided our family in the process of dying from giving
..."Read MoreThe staff at Soulistic were incredible.
The staff at Soulistic were incredible. Bonnie, Camille, Debbie and Jennifer went above and beyondto make sure my mom was comfortable. Their team aided our family in the process of dying from giving us a spiritual counselor to speak with, to giving us the book, “Gone From My Sight: The Dying Experience” by Barbara Karnes, RN, to helping us get an FAA approved oxygen concentrator. They treated my mom as a whole person, acknowledging her own agency and truly caring. I feel our entire healthcare system could benefit from applying the principals and ethics of Soulistic Hospice to the wellness industry. I absolutely recommend this company!Gina
Such A Great Help
Soulistic is taking care of my mom, and I would be lost without them. They are such a great help, and a wonderful group of people. Would recommend to anyone looking for hospice
..."Read MoreSuch A Great Help
Soulistic is taking care of my mom, and I would be lost without them. They are such a great help, and a wonderful group of people. Would recommend to anyone looking for hospice care.Dan H.
Extraordinary Team!
I am grateful to everyone who helped realize my dream for my mother. A comfortable, loving, light, responsive place where all of you can still be with her and provide her with the care she deserves.
..."Read MoreExtraordinary Team!
I am grateful to everyone who helped realize my dream for my mother. A comfortable, loving, light, responsive place where all of you can still be with her and provide her with the care she deserves. She needs this faith-driven organization. Without it I do not believe we would have the same wonderful result.G. Marshall
Kindness and Compassion
Kindness and Compassion
I have never encountered such a team of sentient beings truly dedicated and equally fond of being in service to others. So whether I live another day or ascend to the highest peaks tomorrow makes little difference to me for kindness is strong medicine & Soulistic has assisted me unto a healing path come what may.Tamara
They treat patients like family
Soulistic team members are so caring and compassionate. They treat patients like family. I would highly recommend them to anyone looking to give their family members the very best
..."Read MoreThey treat patients like family
Soulistic team members are so caring and compassionate. They treat patients like family. I would highly recommend them to anyone looking to give their family members the very best care.Hope J.
All the people from Soulistic Hospice really care.
I absolutely love my hospice CNA. She brings joy to me with every visit and helps me with many details that really help to make my life better. I used to do home health care, and there are people
..."Read MoreAll the people from Soulistic Hospice really care.
I absolutely love my hospice CNA. She brings joy to me with every visit and helps me with many details that really help to make my life better. I used to do home health care, and there are people who do it for the money and people who do it because they really care. All the people from Soulistic Hospice really care.Janice V.
Professional and Caring Staff
Soulistic Hospice took care of an elderly family member in my home until she passed. I found their staff to be very caring and professional, and they were always there when we needed them. Their
..."Read MoreProfessional and Caring Staff
Soulistic Hospice took care of an elderly family member in my home until she passed. I found their staff to be very caring and professional, and they were always there when we needed them. Their doctor was exceptional and did regular house calls, which is almost unheard of. I would highly recommend their services to anyone!Vanessa
They helped guide us in the right direction
Soulistic Hospice is the team you want on your side for hospice care! Their whole team consists of caring and knowledgeable wonderful people. They really helped my family and my sister-in-law who was
..."Read MoreThey helped guide us in the right direction
Soulistic Hospice is the team you want on your side for hospice care! Their whole team consists of caring and knowledgeable wonderful people. They really helped my family and my sister-in-law who was dying from cancer. They helped guide us in the right direction for her care, getting us supplies and medicine we needed ASAP and were always available for our concerns and questions. They really care about their patients and the patients' families too. The end of life journey can be very hard and emotional for both patient and family and our family couldn’t have made a better choice with Soulistic. They guided us every step of the way and provided excellent care. I have a new admiration for the hard and caring work these people do!Jennifer T.
I cannot thank you enough.
I cannot thank you enough. Who knew that suchwonderful, selfless angels existed to care for our sick family members when wedidn't know where to turn. This is not a big money hospice, but one full of
..."Read MoreI cannot thank you enough.
I cannot thank you enough. Who knew that suchwonderful, selfless angels existed to care for our sick family members when wedidn't know where to turn. This is not a big money hospice, but one full of compassionate nurses who must be sent from heaven. Thank you for helping us care for my brother. You went out of your way to help us to get him home and to help him to die without pain or discomfort, surrounded by all of his family.John G.
Forever Grateful
Soulistic took beautiful care of my husband, everyone should know about this hospice. I had no idea the blessing they would be to me and my family. The nurses were so compassionate, they are experts
..."Read MoreForever Grateful
Soulistic took beautiful care of my husband, everyone should know about this hospice. I had no idea the blessing they would be to me and my family. The nurses were so compassionate, they are experts at what they do. I don't know how I would have made it through his death if I did not feel that we were in such competent hands. I will never forget them and will forever be so very grateful.Pallora A.
Forever grateful to Soulistic
My family had the great blessing of experiencing the care of Soulistic Hospice for my son’s father at the end of his life. As a result, the last four months of his life were peaceful and surrounded
..."Read MoreForever grateful to Soulistic
My family had the great blessing of experiencing the care of Soulistic Hospice for my son’s father at the end of his life. As a result, the last four months of his life were peaceful and surrounded by love.Karesz was a freedom fighter from Hungary. A veteran and also a beautiful, spiritual man who had suffered greatly in his early life in Europe during and after WW2. Soulistic Hospice actually found an Assisted Living Facility owned and operated by a Hungarian woman who spoke the language fluently and cooked for him the food of his childhood. The entire team from Soulistic Hospice made his last days comfortable. He was especially blessed by his Spiritual Care Coordinator, who was also a veteran and assisted Karesz to make peace with the many painful memories — and to embrace the next stage of his soul journey with joy.I am forever grateful to Soulistic Hospice for going above and beyond the call of duty in caring for every patient and their families. The nurses and CNA’s made Karesz’s physical challenges bearable, and the Social Worker assisted me with making final arrangements efficiently and with caring, patience, and compassion.Kathleen Vasvary
Outstanding service record from Soulistic Hospice
Aslan Assisted Living have an outstanding service record from Soulistic Hospice firm as well as their employees, When we need them, they're always there. The quality of work they do is super! They
..."Read MoreOutstanding service record from Soulistic Hospice
Aslan Assisted Living have an outstanding service record from Soulistic Hospice firm as well as their employees, When we need them, they're always there. The quality of work they do is super! They are on top of medicines as well as accessories needed for our clients. The employees that they have as aides are excellent and they know how to deal very well with behavioral issues.O. Hernandez
Recommending them for almost 10 years
I own Moreno's Assisted Living in Tucson and have very high standards of care. I have recommended Soulistic Hospice to our patients and their families for almost 10 years now and have found them all
..."Read MoreRecommending them for almost 10 years
I own Moreno's Assisted Living in Tucson and have very high standards of care. I have recommended Soulistic Hospice to our patients and their families for almost 10 years now and have found them all to be honest, caring and professional. They are always there when I need them and I only want to work with them for hospice care for my patients. I highly recommend them and their integrity to anyone who needs hospice care for themselves or their loved one.Maria M.
They are the most professional and caring people
I would like to thank Soulistic Hospice for everything they provided for my mom. We could call any time of day or night and get all the support we needed. They are the most professional and caring
..."Read MoreThey are the most professional and caring people
I would like to thank Soulistic Hospice for everything they provided for my mom. We could call any time of day or night and get all the support we needed. They are the most professional and caring people. I appreciate all their caring words during this time. If anyone needs help for their loved ones, we would recommend Soulistic Hospice in a heartbeat. Thank you <3Blanca M.
We Felt Extremely Loved and Supported
I have long been a fan of hospice, but I was swept away by the loving care provided by Soulistic Hospice during the time of my friend's passing. We felt extremely loved and supported! Each person on
..."Read MoreWe Felt Extremely Loved and Supported
I have long been a fan of hospice, but I was swept away by the loving care provided by Soulistic Hospice during the time of my friend's passing. We felt extremely loved and supported! Each person on the team was kind and thoughtful. I can't imagine a more genuine experience than the one my friend had as she passed to the other side.Sandy
The staff truly cared
If you're in need of hospice, the staff at Soulistic, a nonprofit service, offer their expertise healthcare for the patient, not just to earn a paycheck. My husband passed in March 2023 and came home
..."Read MoreThe staff truly cared
If you're in need of hospice, the staff at Soulistic, a nonprofit service, offer their expertise healthcare for the patient, not just to earn a paycheck. My husband passed in March 2023 and came home for the duration of his illness. Soulistic Hospice was at our door the day we got home, with nurses, CNAs, and all the equipment that was needed was delivered the same day. Bedside table, bedside commode, shower chair and medication, then they gave step by step instructions. The staff truly cared with outstanding, professional, certified staff. A 24/7 phone service, and within the hour, a certified nurse is available to help the patient. Even at our door in the middle of the day or night. I can't say enough about Soulistic Hospice. When your family member is at the stage of hospice, call Soulistic Hospice. You will be satisfied. Thank you Soulistic Hospice for all you do. Thank You!!Patricia
Thank You With All My Heart
Soulistic hospice was such a wonderful team. They truly are a blessing. They responded to me right away and were there to provide the care for my Grampa. I'm so grateful for them and I would
..."Read MoreThank You With All My Heart
Soulistic hospice was such a wonderful team. They truly are a blessing. They responded to me right away and were there to provide the care for my Grampa. I'm so grateful for them and I would definitely refer them to whomever would need this kind of care. I thank you with all my heart.Carmelita G.
Best Hospice In Tucson
This is honestly the best hospice in Tucson. We placed my grandma on hospice, and have no regrets using them. They are always so very kind, caring, and professional; from the nurses, medical social
..."Read MoreBest Hospice In Tucson
This is honestly the best hospice in Tucson. We placed my grandma on hospice, and have no regrets using them. They are always so very kind, caring, and professional; from the nurses, medical social worker, chaplains, to their amazing aides, even the office staff, are all meant to do this. I am amazed at how much they have helped us, with things that we didn't even realize we would need help with. If I ever have a concern or question about anything with my grandma and need to call their office, I consistently have someone calling me back to help almost immediately. I am so thankful, I couldn't imagine taking care of my grandma without them and I would never consider anyone else.Allison Z.
The Soulistic staff was excellent
The Soulistic staff was excellent in providing the care my mom needed, taking time to have personal conversations with her, and getting to know my mom. Her nurses, CNAs, and spiritual team all were
..."Read MoreThe Soulistic staff was excellent
The Soulistic staff was excellent in providing the care my mom needed, taking time to have personal conversations with her, and getting to know my mom. Her nurses, CNAs, and spiritual team all were loving and attentive to my mom’s needs. My mom very much appreciated their conversation and friendship. She told me how well each of them took care of her and had patience with her. They communicated with me regularly, kept me abreast of my mom’s health, and advised me of what I could to do to help. I'm ever so grateful for the professionalism of your staff and the personal relationship they had with my mom.C. Reed
Soulistic Hospice Shows Respect for Each Individual in My Home
Soulistic Hospice is a caring hospice. They provide a team to help ensure that individuals and their loved ones are not alone in their journey, so their last days are peaceful and as pain-free as
..."Read MoreSoulistic Hospice Shows Respect for Each Individual in My Home
Soulistic Hospice is a caring hospice. They provide a team to help ensure that individuals and their loved ones are not alone in their journey, so their last days are peaceful and as pain-free as possible. They are a hospice who believes in compassionate care and respect for each individual. I recommend them to everybody!Assisted Living Owner
They were stellar
When my mother's Alzheimer’s was in the later stages Soulistic Hospice became part of my team. They were stellar in their compassionate care, gentle and thorough, on time and understanding. They
..."Read MoreThey were stellar
When my mother's Alzheimer’s was in the later stages Soulistic Hospice became part of my team. They were stellar in their compassionate care, gentle and thorough, on time and understanding. They respected my religious beliefs and were available with counselors for a year after my mom passed. I highly recommend their service!Jennifer T.
Wonderful organization
J. Brown
Answers the phone 24-7
The staff answers the phone 24-7. I've never been in the position to watch a loved one die. They were patient and knowledgeable with answers.The nurse came over after her shift to help me with
..."Read MoreAnswers the phone 24-7
The staff answers the phone 24-7. I've never been in the position to watch a loved one die. They were patient and knowledgeable with answers.The nurse came over after her shift to help me with medication. She explained the dying process with care. I could not have handled my husbands passing with out their assistance.JoAnn H.
Supportive and hands on every step of the way
SOULISTIC Hospice was a bright light that came into my family's life. My mother refused to have anything to do with assisted living and informed me early on that when it came to her long-term care
..."Read MoreSupportive and hands on every step of the way
SOULISTIC Hospice was a bright light that came into my family's life. My mother refused to have anything to do with assisted living and informed me early on that when it came to her long-term care our property was where she was going to finish her days and nowhere else. My mother was the type who declined slowly but surely. It wasn’t drastic until the very end. Our team at SOULISTIC was supportive and hands on every step of the way. They made it very clear to me that their job was to make sure my mother was comfortable and in as little pain as possible. Of course, the last 6 months of a 97-year-old are not easy. Carmen, Bonnie , Christine , Cristina , Gabrielle, Julie and Marj never let us down. I cannot possibly list every person from SOULISTIC who helped my mother on her final journey. There are too many . Fortunately, my mother was a good person. This helped the staff by allowing them to do their job in the most effective way possible. There was a huge amount of respect and kindness coming from every single person involved from the Director of SOULISTIC (Ala'Di) to the people who delivered the meds. I cannot stress enough how important it is to use a non-profit Hospice. This allows the staff to concentrate on the health and well-being of their patients and not on how to make a profit. This philosophy of making the patient comfortable and well cared for was obvious from the beginning to the end. The list of positive experiences goes on and on. There is no doubt in my mind that SOULISTIC Hospice is the number 1 Hospice in Tucson. I cannot think of one negative incident in our time with SOULISTIC. We thank very single person who was involved in my mothers care.Marty S.
They Honestly Care
Soulistic hospice is such a wonderful hospice. We recently had to move my mother in law into our home with us, chose Soulistic because we have heard so many wonderful things about them, and I can now
..."Read MoreThey Honestly Care
Soulistic hospice is such a wonderful hospice. We recently had to move my mother in law into our home with us, chose Soulistic because we have heard so many wonderful things about them, and I can now attest to this ourselves. They have become our partners in caring for her, and have truly become part of our family. They are available whenever we need their help, and the most wonderful part is that they honestly love their jobs. It is so relieving that they are never too busy for our family, they honestly care about all of us, and we have never once felt rushed. I definitely recommend this special company to anyone needing hospice care, we would never go anywhere else.T. Bolton
Very professional
W. Adams
Care and Support was Outstanding
I'm so thankful that Soulistic Hospice was there for both my husband and myself during the last months of his life. The Doctor, Beyana, Aladi, Shureen, Ah'Nuit and everyone at Soulistic were a
..."Read MoreCare and Support was Outstanding
I'm so thankful that Soulistic Hospice was there for both my husband and myself during the last months of his life. The Doctor, Beyana, Aladi, Shureen, Ah'Nuit and everyone at Soulistic were a formidable support team to have working on our behalf. Having knowledgeable, understanding, reassuring guidance was priceless and meant everything to me.Nancy
I most definitely recommend Soulistic
My mom, Alma, passed 10/1/21. During the time she was under the care of Soulistic Hospice, she was treated with respect and kindness by all. Soulistic paired her up with a Navajo CNA, who was
..."Read MoreI most definitely recommend Soulistic
My mom, Alma, passed 10/1/21. During the time she was under the care of Soulistic Hospice, she was treated with respect and kindness by all. Soulistic paired her up with a Navajo CNA, who was wonderful, and I’m sure my mom appreciated that. Also, the nurses working with her made the efforts to call me when needed, and I appreciated that. The Spiritual Care Coordinator was very kind and called numerous times to pray with her and provide spiritual support. All of these services helped her and me to deal with the end of her life more gracefully and positively. Thank you all. I most definitely recommend Soulistic Hospice services to anyone looking for all-encompassing healthcare for life ending.Yolanda B.
So Happy We Found Them!
So Happy We Found Them!
Soulistic Hospice really work together as a team to educate, guide and understand all aspects of what they do and what to expect during this trying time of our lives. We are very happy we found them!R. Martinez
Soulistic Hospice Has Been a Breath of Fresh Air for Our Assisted Living Home and Our Residents
Soulistic Hospice Has Been a Breath of Fresh Air for Our Assisted Living Home and Our Residents
Soulistic Hospice services has been a 'breath of fresh air' for our Assisted Living Home and our residents. We felt our residents and their families were just another cold emotionalized number to other hospices we had tried. Soulistic Hospice has provided that loving touch and compassion.Adult Care Home manager, Tucson, AZ
Kind, considerate, loving, respectful
My Dad only had hospice care for a week and a half before his passing. I had the pleasure of meeting them all. They were kind, considerate and the most loving and respectful ladies. They treated
..."Read MoreKind, considerate, loving, respectful
My Dad only had hospice care for a week and a half before his passing. I had the pleasure of meeting them all. They were kind, considerate and the most loving and respectful ladies. They treated my father so kindly. I will forever be in their debt.Carole K.
Soulistic is an incredibly team.
I cannot say enough positive things about Soulistic Hospice. The process of dying is never easy for any family, but ours was especially difficult – and they were there for us every step of the way.
..."Read MoreSoulistic is an incredibly team.
I cannot say enough positive things about Soulistic Hospice. The process of dying is never easy for any family, but ours was especially difficult – and they were there for us every step of the way. Our daughter was only 18, and other providers in town denied her care, saying it would be too emotionally difficult for their staff. In contrast, our nurse and the entire Soulistic team were incredibly supportive, compassionate and fully engaged. We were so impressed with their service. I would wholeheartedly recommend Soulistic Hospice to anyone in need of hospice care.Anonymous
God Bless This Company!
I love this hospice company! I needed help urgently with my live in grandmother and they came out to my home within two hours with equipment, medication and nursing help. They came out every day
..."Read MoreGod Bless This Company!
I love this hospice company! I needed help urgently with my live in grandmother and they came out to my home within two hours with equipment, medication and nursing help. They came out every day because of her illness and confusion. I literally would never recommend any other company in the Tucson area. They saved me and she had a wonderful Christian counselor. God bless this company!Cindi
I highly recommend them!
Soulistic Hospice provided excellent care to one of my family members. They were sensitive to our cultural needs and went above and beyond our expectations. They have competent and compassionate
..."Read MoreI highly recommend them!
Soulistic Hospice provided excellent care to one of my family members. They were sensitive to our cultural needs and went above and beyond our expectations. They have competent and compassionate staff on call 24 hrs a day 7 days a week, which made my family feel very secure. I highly recommend them!!M. Ikwe
Love & Guidance
I used to work for Soulistic. It was the last nursing job I have ever had before retirement, and by far the most wonderful, they accepted me with open arms. I loved this job more than any place I
..."Read MoreLove & Guidance
I used to work for Soulistic. It was the last nursing job I have ever had before retirement, and by far the most wonderful, they accepted me with open arms. I loved this job more than any place I have ever worked as a nurse. Each of the people that I worked with had individual gifts that were allowed to flourish. I received nothing but love and guidance to care for our beautiful patients and their needs. I know that I will call Soulistic whenever I believe that my time is near.Judith B.
They were there for us when others weren't
My mother went on hospice on her 90th birthday and was dropped ten days later by another hospice organization because of her insurance. Soulistic Hospice stepped right in and took extraordinary
..."Read MoreThey were there for us when others weren't
My mother went on hospice on her 90th birthday and was dropped ten days later by another hospice organization because of her insurance. Soulistic Hospice stepped right in and took extraordinary compassionate, professional, and loving care of my mother until the very end. They were available 24/7, she had regular visits from the nursing staff, the pastor, and the attending physician. I was incredibly impressed by their professionalism, sensitivity, willingness to serve, and truly compassionate loving care. As a psychotherapist for over 30 years in Tucson I will only recommend Soulistic Hospice and the Care Homes they service.Susan W.
Soulistic provided the best that hospice can offer
Signing up with Soulistic Hospice was the best decision for our family as our mother’s health declined over the past few years. The care that she received contributed to her being able to maintain a
..."Read MoreSoulistic provided the best that hospice can offer
Signing up with Soulistic Hospice was the best decision for our family as our mother’s health declined over the past few years. The care that she received contributed to her being able to maintain a good quality of life, which was most important to her and to us. Mom really wanted to stay at home, and Soulistic staff provided what she needed while also keeping us informed and comforted. The nurses who checked Mom’s health gave us enough details without overwhelming us. The CNAs who came in daily became part of the family, demonstrating amazing care and kindness. They all recognized Mom’s sense of humor and made sure that she always looked nice, as that was also important to her. All the staff were very responsive whenever we had questions or needed more information. Overall, Soulistic provided the best that hospice services can offer and we are grateful that, with their help, we honored our mother’s wishes to experience a peaceful ending to her life.C. Sax
They are angels
There are no words to express how thankful we are for this company. After years of battling lung cancer, we were given a terminal diagnosis for my mother and were referred to Soulistic Hospice to
..."Read MoreThey are angels
There are no words to express how thankful we are for this company. After years of battling lung cancer, we were given a terminal diagnosis for my mother and were referred to Soulistic Hospice to help care for her. To say that they helped us through her death is not giving justice to what we experienced with them. They were at our home every single day at the end, holding her hand, teaching us what was going on and what to expect next, and helping us to make the right decisions to care for her. They are angels, I don't know how they found so many wonderful people in one single company, but they are the better than we could have ever hoped for.Radiogog P.
Incredibly Supportive
I am so grateful for Soulistic Hospice and the care that they are providing to my mother. The staff is incredibly supportive, kind and quick to respond. They've treated my mom with the upmost respect
..."Read MoreIncredibly Supportive
I am so grateful for Soulistic Hospice and the care that they are providing to my mother. The staff is incredibly supportive, kind and quick to respond. They've treated my mom with the upmost respect and dignity during this time. I'm glad I chose Soulistic for my mother and 100% recommend their services to anyone. Your loved one will be in the best of hands.Blanca D.
Highly Recommended!
Soulistic Hospice took care of a dear friend of mine. The attention to detail, and the expedited methods used to ensure delivery of equipment and medications were excellent. The nursing staff, their
..."Read MoreHighly Recommended!
Soulistic Hospice took care of a dear friend of mine. The attention to detail, and the expedited methods used to ensure delivery of equipment and medications were excellent. The nursing staff, their heartfelt support, along with their availability after hours was a God send, during a very difficult time. I would highly recommend this company to anyone in need!Laura G.
Forever indebted to Soulistic Hospice
Even at my ripe old age of 83, I knew very little about Hospice, didn’t think I wanted to know much about it, and obviously did not want to be in a position where I needed it. But, as my wife was
..."Read MoreForever indebted to Soulistic Hospice
Even at my ripe old age of 83, I knew very little about Hospice, didn’t think I wanted to know much about it, and obviously did not want to be in a position where I needed it. But, as my wife was nearing the end of her battle with cancer, I reached out to friends, relatives, and former users of Hospice for their input and advice. Everything I read, learned, and heard pointed me in the direction of a non-profit.As soon as I contacted Soulistic Hospice in Tubac, all my fears and concerns dissipated, and I knew I had made a perfect choice. Throughout the entire process of life’s fragile ending, my wife and I received nothing but the most professional and loving support and care available. Every facet of service, from nursing, caretaking, and spiritual, were provided with care, promptness, and love. I will be forever indebted to Soulistic Hospice.D. McLean
Top notch care and support!
From my first phone call to months of top notch care and support I am so happy that I switched to Soulistic Hospice. It has made a huge difference in many lives surrounding one
..."Read MoreTop notch care and support!
From my first phone call to months of top notch care and support I am so happy that I switched to Soulistic Hospice. It has made a huge difference in many lives surrounding one person.Karen S
Best company in Tucson
I have had excellent service and I highly recommend them. When it comes to the point your love ones are getting ready to pass this is by far the best company in Tucson. They are caring understanding
..."Read MoreBest company in Tucson
I have had excellent service and I highly recommend them. When it comes to the point your love ones are getting ready to pass this is by far the best company in Tucson. They are caring understanding and very professional.V. Leibowitz
The best single choice
Choosing this hospice was the best single choice that we could have made for my grandmother. The nurses were compassionate and always available to us. Our questions were always answered thoroughly,
..."Read MoreThe best single choice
Choosing this hospice was the best single choice that we could have made for my grandmother. The nurses were compassionate and always available to us. Our questions were always answered thoroughly, and we never felt that we were alone. Thank you so much to this wonderful company for guiding us through this difficult time.P. Bollen
The best service we have received.
Soulistic Hospice has been the best service we have received. I cannot exclude any of the staff. Nurses, CNAs, social services are so professional and passionate of their work. Francis is very caring
..."Read MoreThe best service we have received.
Soulistic Hospice has been the best service we have received. I cannot exclude any of the staff. Nurses, CNAs, social services are so professional and passionate of their work. Francis is very caring and so kind. My husband and I always look forward on seeing her. She puts a smile on my husband. I want to include Griselda, Belen, Lorena Chavez, Sylvia, Karene, Arlene, Francis. They are ANGELS. Thank you Soulistic Hospice for being the best company in Nogales.Cathy P.
I would recommend you to anyone
Verla
Letter from family
Dear Hospice Staff, I want to convey my deepest gratitudefor the exceptional care Soulistic Hospice provided my mother in the period before her passing. The care and love you provided for my mother
..."Read MoreLetter from family
Dear Hospice Staff, I want to convey my deepest gratitudefor the exceptional care Soulistic Hospice provided my mother in the period before her passing. The care and love you provided for my mother in her final moments was exceptional. My mother, who greatly appreciated the companionship and care of those around her, constantly spoke of many of you. My mother held a special place in her heart for Marisela, her CNA. She genuinely looked forward to Marisela's visits, and the comfort and joy she brought during those moments were immeasurable. Marisela, your care was a bright spot in my mother's days, and I can't thank you enough for the genuine warmth and attention you showed her.Sylvia, your professionalism and compassion left an indelible mark on my mother's heart. She admired you deeply and always spoke about how fortunate she was to have you by her side. Thank you for being a pillar of strength and solace for her.Lorena, your compassion and understanding were like a soothing balm to my wounded soul. You provided me with a shoulder to lean on, a listening ear, and a comforting presence when I needed it the most. Your kindness and empathy helped me navigate the depths of grief, and I will always remember your unwavering support.Arlene, your compassionate and empathetic approach helped me navigate the complex emotions and decisions that came with my mother's illness and eventual passing. You listened without judgment, provided invaluable advice, and helped me find the resources and support I needed.I also want to express my gratitude to all the RNs who came to visit. Each one of you played a vital role in my mother's care and well-being. You all contributed to making her last months as comfortable and dignified as possible. My mother felt loved and cared for by her entire hospice team, and that meant the world to her and to us, her family.I'd also like to extend a heartfelt thank you to Ala’Di. Your compassion and empathy were evident in every word and gesture, and your expertise and experience were invaluable in helping me navigate the complexities of those final hours. Your support not only eased my mother's transition but also provided me with the emotional strength to be there for her until the end.While my mother is no longer with us, I find solace in knowing that she received the best possible care in her final days. Your team's professionalism, compassion, and unwavering support made all the difference. You not only cared for her physical needs but also provided emotional comfort to our entire family.Please accept my sincerest appreciation for your dedication and the exceptional care you gave to my mother. Your kindness during this challenging time will always be remembered, and you will forever hold a special place in our hearts.With heartfelt thanks,Lilliana A. and FamilyLilliana A. and Family
I highly recommend Soulistic Hospice!
I can’t express how grateful I am to have found Soulistic Hospice to help with medical care, advice and support for my husband. Our nurse has been a blessing and a remarkable resource for me. She is
..."Read MoreI highly recommend Soulistic Hospice!
I can’t express how grateful I am to have found Soulistic Hospice to help with medical care, advice and support for my husband. Our nurse has been a blessing and a remarkable resource for me. She is so knowledgeable, professional and truly caring! I couldn’t have navigated through this difficult time without her! Soulistic Hospice is an amazing organization with excellent service that goes above and beyond for patients. I highly recommend Soulistic Hospice!Linda D.
I quickly realized that the choice of Soulistic Hospice for my wife’s care was the right choice.
Thank you Soulistic Hospice and your team members. I would like to take this opportunity to thank the entire team at Soulistic Hospice. The very first night my wife, who had ALS, was placed on
..."Read MoreI quickly realized that the choice of Soulistic Hospice for my wife’s care was the right choice.
Thank you Soulistic Hospice and your team members. I would like to take this opportunity to thank the entire team at Soulistic Hospice. The very first night my wife, who had ALS, was placed on hospice she had a severe breathing attack. The response to my call for help was almost immediate. First a nurse, then a respiratory therapist with oxygen came to our home. My wife was made very comfortable in a short period of time. I quickly realized that the choice of Soulistic Hospice for my wife’s care was the right choice. Subsequent visits form nurses, therapists and aides at our home were very caring, loving, and dedicated to providing the best care for my wife. This made it much easier to cope with the difficult situation that I was experiencing. The staff was also concerned about my health and welfare and provided me with as much needed information and support as possible. I highly recommend Soulistic Hospice.The Duke
We Are Greatly Appreciative!
After my wife returned home from the Rehabilitation Center and was given the diagnosis of COPD, Soulistic Hospice entered the picture. My wife was greatly impressed and was much more comfortable. At
..."Read MoreWe Are Greatly Appreciative!
After my wife returned home from the Rehabilitation Center and was given the diagnosis of COPD, Soulistic Hospice entered the picture. My wife was greatly impressed and was much more comfortable. At 90 years old, I was very relieved. It gave my wife such happiness and a few months of quality living. We are greatly appreciative!Don
They genuinely care for you.
The word Hospice is immediate fear for all ears, but Soulistic Hospice provides the connection of Body and Soul that is so comforting for all. They are professional in all the caring and loving
..."Read MoreThey genuinely care for you.
The word Hospice is immediate fear for all ears, but Soulistic Hospice provides the connection of Body and Soul that is so comforting for all. They are professional in all the caring and loving services they provide. The patient is given a sense of peace as well as the loved one caring for the patient. You find the Soul as important as the general medical only approach. They do more than provide care for the patient. They genuinely care for you and the patient. That caring continues after your loved one has passed on. Soulistic Hospice is my only choice when hospice care is needed.J. Hubbard
They truly are a blessing!
The staff, whether it was the nurses, CNA's or even the office staff, was so caring and understanding. They never got frustrated when I called because I was unsure of something or asked a million
..."Read MoreThey truly are a blessing!
The staff, whether it was the nurses, CNA's or even the office staff, was so caring and understanding. They never got frustrated when I called because I was unsure of something or asked a million questions when they came to our house to check on our loved one. You can tell what they do and they treated my loved one just as though it was theirs. They truly are a blessing!Aubree G.
My mother was very well taken care of.
My mother was very well taken care of, the team would answer the phone immediately, medication was provided same day or early morning, great people with lovely hearts and care for the patient and the
..."Read MoreMy mother was very well taken care of.
My mother was very well taken care of, the team would answer the phone immediately, medication was provided same day or early morning, great people with lovely hearts and care for the patient and the family, my mom passed away comfortable in her bed with no pain.¡We-Silly!
Loving Attention and Kind Staff
I had the good fortune to work closely with this fine dedicated hospice team. Because my friend needed care around the clock, the Soulistic team went the extra mile and helped us to assemble and
..."Read MoreLoving Attention and Kind Staff
I had the good fortune to work closely with this fine dedicated hospice team. Because my friend needed care around the clock, the Soulistic team went the extra mile and helped us to assemble and coordinate a quality caregiving team. Without them, we would not have known where to start.William
Very pleased
Very pleased
The nurses are great, our CNA is wonderful, our supplies always arrive on time, the staff always return my calls. We get a nurse right away when we need one. I am very pleased with them and highly recommend them.Jackie M.
Soulistic Hospice stood out.
I interviewed multiple hospice services in Tucson; Soulistic Hospice stood out as the only one capable of meeting my mom's needs. They differentiate themselves by working as a team, treating patients
..."Read MoreSoulistic Hospice stood out.
I interviewed multiple hospice services in Tucson; Soulistic Hospice stood out as the only one capable of meeting my mom's needs. They differentiate themselves by working as a team, treating patients as individuals, and offering a holistic approach to end-of-life care. From the intake team to nurses and counselors, they are highly skilled, compassionate, and responsive to patient and family needs.They are true earth angels,and I am grateful for their support in such a difficult time.Nora V.
October 9, 2020
Soulistic Hospice 18
Calle Iglesia Tubac, AZ 85646
Attn: Ms. Goodman,
Thank you to Soulistic Hospice and your team members.
I would like to take this opportunity on behalf of the Zepeda Family thanks all of the team at the Soulistic Hospice Program.
On June 2020, my mother in law after being released from the hospital was placed in hospice. From the time that she was placed in hospice, we were informed that her health would begin to deteriorate and that she had between 1 month and 2 years to live. My wife was provided with telephone numbers to several hospice programs whom service the Santa Cruz County area. We were asked to request information from each of the companies to make a decision as to who would help us take care of my mother in law in her finally stages of life. This was an extremely difficult decision to make.
While talking to various people, we were informed that Soulistic Hospice had some very dedicated people working for their program whom provided a higher level of care than any other program in the state of Arizona. Some of the people who provided this information are people who themselves work for both the State of Arizona, people whom loved ones have been cared for by Soulistic Hospice, Doctors in the Santa Cruz County Community, and Doctors/Nurses for the hospital where my mother in law was attended to in Tucson, Arizona. After contacting the different programs and making the difficult decision, my wife chose to contact Soulistic Hospice. From the moment we picked up the phone and spoke to your social worker, we noticed the level of care that your company provides. She was compassionate and very informative about the program and the level of care that the program provided. She explained to my wife and I, how the program worked, what was provided and how the team would care for my mother in law at our home. She explained what to expect and told us that we could pick up the phone at any time and ask for guidance if we had any questions.
When we met your nurses at our home for the first time, both were very caring, loving, and dedicated to providing the best care for my mother in law. Throughout the care of my mother in law, they also showed the level of professionalism and compassion they felt for she and my family. By far they treated my mother in law as if she was their own grandmother, parent, or sibling during this time. Both were exceptional in their care.
When it comes to your CNA, the words that come to mind which best describe her are compassionate, loving, caring, dedicated, and most than anything professional. She took care of my mother in law as if she was her own mother. Her always happy attitude brings out the best person in her and made these difficult times easier. She would always tell us what to expect and is willing to help and take exceptional care of her patients.
There were times that both your nurse and CNA would call on their days off just to ask how my mother in law was doing or if we needed anything. They were always interested in knowing how she had awoken and if she was doing well. Not only were they concerned about her but they too were concerned about how my wife was doing. They would continuously ask her if she needed anything and if she was okay. They would always offer her help if needed.
All of the Soulistic Hospice employees whom cared for my mother and law brought the name of Soulistic Hospice to a higher professional level. The Zepeda family is extremely thankful with your employees and Soulistic Hospice because in these difficult times, you all made it easier to cope with the much difficult times that we were experiencing.
Thank you for everything you did for our family during these times. We now know that we made the best decision by contacting Soulistic Hospice.
Respectfully,
The Zepeda Family

Ala'Di Goodman, RN
Executive Director
Director of Clinical Services
Interfaith Minister
Human-Rights Advocate

Ala'Di Goodman, RN
Executive Director
Director of Clinical Services
Interfaith Minister
Human-Rights Advocate
Ala'Di was born and raised in Christchurch, New Zealand and received her diploma as a comprehensive registered nurse in 1993. Her nursing experience encompasses a variety of healthcare fields including psychiatric, post-partum, geriatric, orthopedic, rehabilitation, home health, and hospice care. Ala'Di is an educator in her field of expertise to both public and professional audiences. She is intuitive and sensitive to both patients and their loved ones and has dedicated her life to serving humanity. Ala'Di is also a musician and artist and has a love of animals.
TUCSON, AZ, November 17, 2022 – Ala’Di Goodman has been inducted into Marquis Who’s Who. As in all Marquis Who’s Who biographical volumes, individuals profiled are selected on the basis of current reference value. Factors such as position, noteworthy accomplishments, visibility, and prominence in a field are all taken into account during the selection process.
Ms. Goodman is a Registered Nurse and the Executive Director of Soulistic Hospice, a nonprofit institution for which she has worked since 2008. She considers her position a calling – more than just a job – and through it, she provides the highest quality end-of-life care. Ms. Goodman has enjoyed a long tenure with Soulistic Hospice, which has offices in both Tucson and Tubac, Arizona and serves two counties, including as the director of admissions, the director of clinical services, and the director of community outreach.
A native of New Zealand who immigrated to the United States in 1994, Ms. Goodman received a comprehensive registered nurse diploma at Christchurch Polytechnic Institute of Technology in 1993, a premier institution for nurse training. She also gained valuable experience across various health care disciplines, including psychiatry, women’s health, rehabilitation, and geriatric care, all of which contribute to her holistic approach to serving patients.
Working with the nonprofit Soulistic Hospice is energizing and motivating for Ms. Goodman; she proudly collaborates with colleagues to deliver superior patient care. Ms. Goodman credits her success to the guidance and support of superb mentors and her commitment to pursuing personal and spiritual growth and service to humanity. Through hospice care and beyond, she is eager to continue tending to patients’ health care and supporting individuals with their broader emotional and psychospiritual needs, and to helping build a sustainable future of unity and global peace.
About Marquis Who’s Who®:
Since 1899, when A. N. Marquis printed the First Edition of Who’s Who in America®, Marquis Who’s Who® has chronicled the lives of the most accomplished individuals and innovators from every significant field of endeavor, including politics, business, medicine, law, education, art, religion and entertainment. Today, Who’s Who in America® remains an essential biographical source for thousands of researchers, journalists, librarians and executive search firms around the world. Marquis® publications may be visited at the official Marquis Who’s Who® website at www.marquiswhoswho.com.

Dr. Nelson Sandoval, MD
Medical Director
Director médico

Dr. Nelson Sandoval, MD
Medical Director
Director médico
Dr. Nelson Sandoval, MD graduated from Universidad Autonoma De Guadalajara, Facultad De Medicina and specializes in internal medicine. He has been serving the Tucson community since completing a residency with the Tucson Hospital Medical Education Program. Dr. Sandoval joined the Soulistic team in 2018 and is fluent in Spanish.
Dr. Nelson Sandoval, MD se graduó de la Universidad Autónoma de Guadalajara, Facultad De Medicina y se especializa en medicina interna. Ha estado sirviendo a la comunidad de Tucson desde que completó una residencia en el Programa de Educación Médica del Hospital de Tucson. El Dr. Sandoval se unió al equipo de Soulistic en 2018 y habla español con fluidez.
Frequently Asked Questions
Here you'll find answers to the most common questions people ask when considering hospice care.
We welcome all questions about our services, so feel free to contact us at any time.
Click the arrows to view answers.Medicare, AHCCCS (Medicaid), and most private insurance plans cover the cost of hospice care. If you do not have any insurance coverage, we will work with you and your family to ensure you get the services you need. We serve everyone regardless of ability to pay.
Hospice can help to manage the physical, emotional, and spiritual needs of the patient and family or caregivers and includes routine visits to your home or facility by a physician, Registered Nurse, Certified Nursing Assistant, Social Worker, Chaplain, Bereavement Coordinator, and Volunteers.
Hospice also provides medical equipment as well as incontinent supplies and medications to keep your loved one or patient comfortable. Hospice services are 100% covered by Medicare and most private insurances. Soulistic Hospice is a nonprofit organization and strives to provide quality hospice care regardless of ability to pay.
The federal Medicare Hospice Benefit is covered under Medicare Part A. The Benefit covers virtually all aspects of hospice care with very little, if any, out-of-pocket expenses to the patient or family. Soulistic Hospice is fully certified by Medicare.
Medicare covers these hospice services:
- Hospice physician services
- Nursing care
- Medical equipment (including hospital beds, wheelchairs, and walkers)
- Medical supplies (including briefs, wipes, oxygen, bandages, catheters and much more)
- Medications for managing symptoms and controlling pain
- Home health aide services
- Social workers
- Dietary counseling
- Grief support for patients and families
Eligibility for hospice care is determined by your insurance carrier; for Medicare patients, eligibility begins when your doctor determines you have six months left to live. Because doctors often do not refer patients to hospice care services until mere weeks or days before death, we encourage you to discuss it with your doctor when you are first diagnosed with a life limiting condition. Doing so will help ensure that you receive all the benefits of hospice care for the full period you're eligible.
Hospice care includes an integrative approach and does not replace medical treatment, nor does it hasten or delay the end of life. Our team of professional caregivers includes nurses, doctors, and other medical professionals such as social workers, home health aides, grief counselors, Interfaith ministers, trained volunteers, and more. Together, we meet all of your emotional, medical, spiritual, and physical needs. Soulistic Hospice care is more focused on improving your quality of life, providing comfort-oriented care, and preserving dignity.
If your loved one is experiencing any of the following signs or symptoms, it may be time to call and see if they qualify for additional care.
- Uncontrolled or increased pain
- Frequent infections
- Frequent visits to the doctor's office or hospital
- Shortness of breath
- Needs oxygen
- Increased confusion
- Uncontrolled nausea/vomiting or diarrhea
- Frequent falls
- Losing weight and/or interest in food
- Difficulty swallowing and/or choking on food
- Increased weakness and sleeping
- Requires more assistance with daily care
- Has a life limiting illness such as heart, pulmonary, kidney or liver disease, or cancer
- Has chronic health conditions such as diabetes, dementia, Parkinson's disease, or stroke
Yes, hospice is a 24 hour service.
Yes, hospice is a 24 hour service.