Navigating the complexities of end-of-life care can be deeply emotional and overwhelming for patients and their families. Hospice care offers comfort and dignity during this challenging time, focusing on improving quality of life rather than pursuing curative treatments. However, how do healthcare professionals determine the right time to begin these conversations? That’s where the Surprise Question comes in.
If you’re interested in learning about the role of the Surprise Question in hospice care, this guide will dive into the details. By the end, you’ll have a clearer picture of this screening tool and the next steps to take if your loved one may benefit from hospice care.
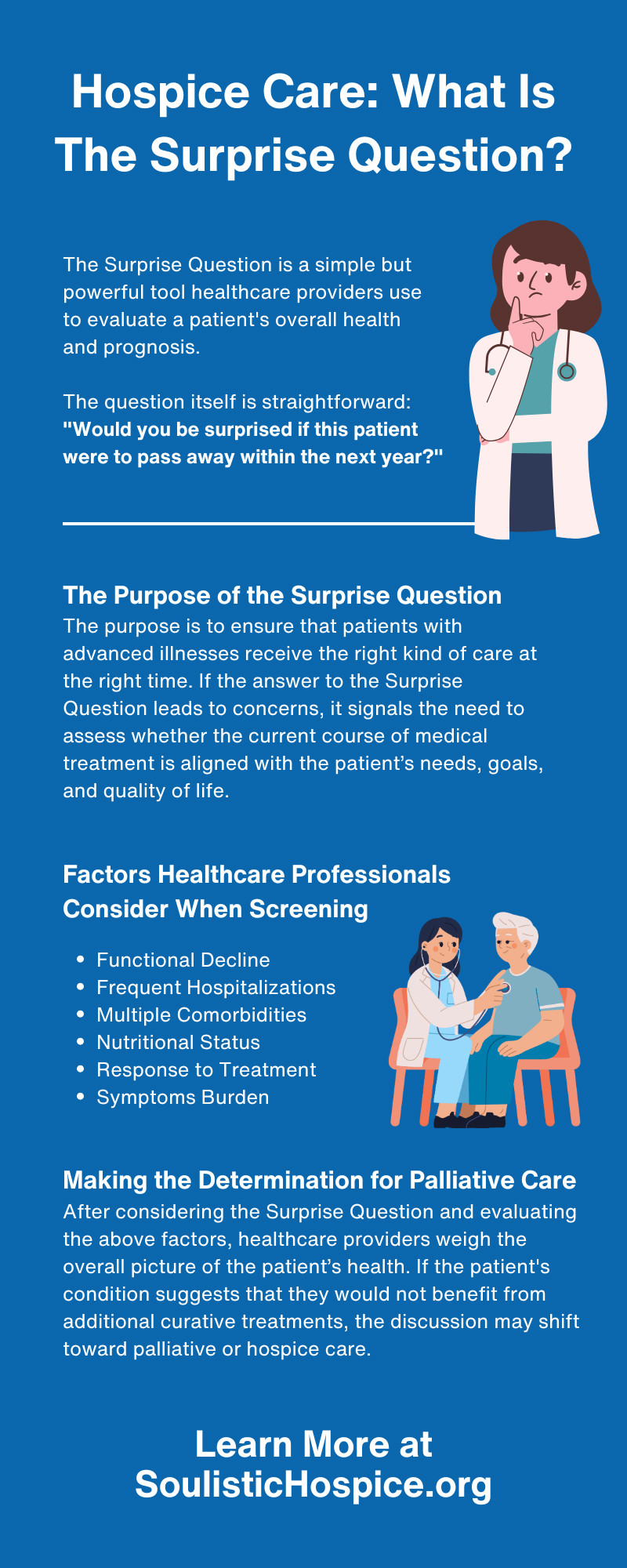
Understanding the Surprise Question Screening Tool
The Surprise Question is a simple but powerful tool healthcare providers use to evaluate a patient’s overall health and prognosis. The question itself is straightforward:
"Would you be surprised if this patient were to pass away within the next year?"
While it may seem like a simple yes or no question, the answer provides valuable insights into a patient’s condition and whether palliative care or hospice support should be considered. The question is not about predicting exact timelines but assessing the likelihood of a patient’s decline based on their current health status.
This screening tool is commonly used in medical discussions to identify patients who might benefit from additional care focused on comfort, symptom management, and emotional support.
The Purpose of the Surprise Question
The Surprise Question serves a crucial role in determining whether a patient might be eligible for palliative or hospice care. It stands apart from technical diagnostic tests or detailed prognostic calculations because it considers clinical judgment and intuition. When healthcare professionals feel they wouldn’t be surprised by a decline within the next year, exploring the possibility of shifting from curative treatments toward supportive care is often a prompt.
The purpose is to ensure that patients with advanced illnesses receive the right kind of care at the right time. If the answer to the Surprise Question leads to concerns, it signals the need to assess whether the current course of medical treatment is aligned with the patient’s needs, goals, and quality of life.
Factors Healthcare Professionals Consider When Screening
When deciding whether hospice or palliative care may be appropriate, healthcare providers consider various factors alongside the Surprise Question. These factors paint a fuller picture of a patient’s overall health and potential trajectory.
Functional Decline
One of the first things healthcare professionals look for is whether a patient is experiencing functional decline. This includes assessing their ability to perform daily activities such as dressing, eating, or moving about independently. If a patient’s physical or cognitive skills are steadily diminishing, it could indicate worsening health and the need for supportive care.
Functional decline is often gradual, making it an essential indicator for providers to monitor over time. Family members may notice subtle changes, like difficulty climbing stairs or remembering appointments, that point to an overall decline in independence.
Frequent Hospitalizations
Repeated hospital visits for the same or worsening condition can be a red flag in a patient’s care timeline. If a loved one has been admitted to the hospital multiple times in recent months, this may indicate that treatment is less effective than hoped and that their overall prognosis is poor.
Frequent hospitalizations place physical and emotional stress on patients and their families. Moving toward hospice care can provide a more supportive environment, reducing the need for repeated emergency visits and focusing instead on making patients comfortable.
Multiple Comorbidities
Comorbidities refer to the presence of multiple chronic conditions, such as diabetes or chronic obstructive pulmonary disease (COPD), for example. These conditions can compound one another, making it harder for the body to recover or sustain critical functions.
When multiple illnesses work together to weaken the body, healthcare providers consider whether focusing solely on comfort might be a better path forward. The goal is not just to address one condition but to provide holistic care that meets the patient’s entire range of needs.
Nutritional Status
Patients facing advanced illness often experience unintentional weight loss or signs of malnutrition. A poor nutritional status can indicate that the body is struggling to maintain essential functions, even with adequate medical intervention.
Losing the ability or desire to eat is a key factor in determining the need for hospice or palliative care. Providers may assess nutritional intake during discussions around shifting care priorities.
Response to Treatment
If a patient is no longer responding to medical treatment, this is often a significant turning point in their care plan. When therapeutic options no longer yield meaningful improvements, it may be time to consider transitioning to care that prioritizes the patient’s comfort and dignity.
Recognizing when treatments are failing allows patients and families to refocus their efforts on making the most of their remaining time together, rather than enduring further medical interventions.
Symptoms Burden
Patients nearing the end of life often experience significant symptom burdens, such as severe pain, breathlessness, or fatigue. These symptoms can dramatically reduce quality of life, making daily activities and social interactions more challenging.
By evaluating the severity of symptoms, healthcare providers can determine whether a patient might benefit from palliative care focused on easing discomfort and improving their overall well-being.
Making the Determination for Palliative Care
After considering the Surprise Question and evaluating the above factors, healthcare providers weigh the overall picture of the patient’s health. If the patient’s condition suggests that they would not benefit from additional curative treatments, the discussion may shift toward palliative or hospice care.
The decision to explore hospice care is not one made lightly. The process is collaborative, involving patients, their families, and the care team, all focused on prioritizing the patient’s needs and wishes. The goal is to make the transition to supportive care as compassionate and seamless as possible.
Next Steps to Take
If your loved one has been identified as eligible for hospice or palliative care, there are actionable steps you can take to ensure they receive the best care and support:
- Talk with a Hospice Provider: Reach out to a trusted hospice organization like Soulistic Hospice to understand options for care and how to get started.
- Gather Medical Records: Ensure all relevant medical records and prescriptions are ready for the hospice team to review. This ensures a smooth transition of care.
- Have an Open Discussion: Speak with your loved one about their wishes and priorities. Open communication is essential for aligning care with their goals.
- Explore Emotional Support Options: Hospice care often includes family counseling and bereavement services. Take advantage of these resources to support both patients and caregivers.
Hospice Care Provides Comfort and Support
Understanding the role of the Surprise Question in hospice care and its role in determining eligibility can empower families to make informed, compassionate decisions about the care they provide their loved ones. Choosing hospice is about choosing comfort, dignity, and quality of life.
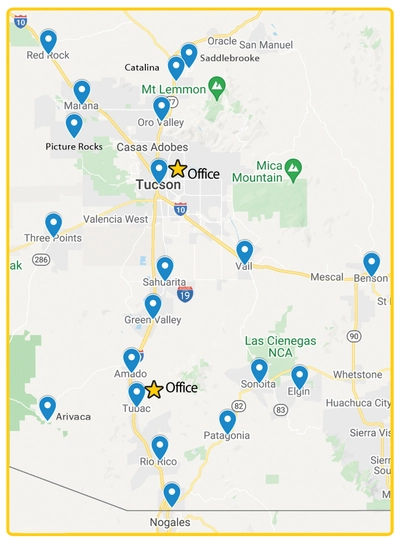
If you want to learn more about hospice in Tucson, AZ, contact Soulistic Hospice today. Our team is here to support your family with warmth, compassion, and unparalleled expertise in hospice care.