Proper nutrition is crucial at every stage of life, but it becomes especially important as an individual nears the end of their journey. For people facing terminal illnesses and their loved ones and caregivers, understanding the role of nutrition can make a significant difference in quality of life during this challenging time. We’ll explore the things to know about nutrition near the end of life, providing practical guidance for ensuring the best possible care.
Understanding Nutritional Needs at the End of Life
As individuals approach the final stages of life, their bodies undergo significant changes, necessitating a corresponding shift in nutritional needs. One of the most noticeable changes is a slowdown in metabolism, which directly affects the body’s capacity to process and absorb essential nutrients efficiently. This metabolic deceleration can be attributed to reduced physical activity and the natural decline in bodily functions associated with aging.
Caregivers and healthcare providers must recognize these physiological changes and understand that traditional dietary recommendations may no longer be suitable. Adapting dietary approaches to accommodate these shifts is essential for maintaining the health and well-being of individuals in their final life stages.
The Role of Diet in Quality of Life
Nutrition is crucial for maintaining physical health and significantly impacts emotional well-being and overall quality of life. Enjoying meals, especially when shared with loved ones, can offer profound comfort, evoke pleasure, and instill a sense of normalcy and connection during challenging times. Such moments allow for emotional respite and foster social bonds, enriching our lives beyond the mere nutritional value of food.
Therefore, it's important to strike a delicate balance between meeting one's nutritional needs and prioritizing the individual's preferences, desires, and the joy of culinary experiences. Recognizing the multifaceted role of nutrition can help nurture both the body and soul, emphasizing that what we eat sustains us physically, supports our emotional health, and contributes to a fulfilling life.
Common Nutrition Concerns
Several issues frequently arise when it comes to nutrition near the end of life, making it a complex area of care. These challenges can include reduced appetite, difficulty swallowing, and the body's decreased ability to process nutrients. Understanding and addressing these issues is crucial for ensuring the comfort and well-being of individuals during this sensitive period. Some of these concerns include:
- Loss of appetite: As the body's needs change, individuals may experience a decreased desire to eat.
- Difficulty swallowing: Some conditions can make swallowing food and liquids challenging or painful.
- Dehydration: Decreased fluid intake and side effects of medications can lead to dehydration.
Strategies for Handling These Concerns
Several effective strategies exist for managing nutritional concerns near the end of life, each designed to address specific issues and enhance patients' overall outcomes. These comprehensive strategies aim to ensure that nutritional needs are met in a manner that respects the individual's comfort and preferences, ultimately contributing to a better quality of life in their final days.
- Offer smaller, more frequent meals and snacks.
- Prepare soft, easy-to-swallow foods.
- Use thickeners for liquids if swallowing is a problem.
- Encourage fluid intake through soups, popsicles, and other sources.
- Consider nutritional supplements or fortified foods.
The Role of Caregivers and Family in Nutritional Support
Caregivers and family members are crucial in ensuring the nutritional well-being of their loved ones, playing a pivotal role in supporting their dietary needs. This entails preparing healthy meals and ensuring that the food is appealing and tailored to the individual's specific health conditions or dietary restrictions.
It may also be necessary to assist with feeding, monitor food intake for any signs of malnutrition or dehydration, and adjust the diet based on feedback from a healthcare professional. Their involvement is key to promoting a balanced and nutritious diet, essential for the overall health and recovery of the person they care for.
Practical Advice for Providing Nutritious Meals
Providing nutritious meals near the end-of-life stage is absolutely crucial. Adhering to a nutrition plan tailored to the individual's specific needs is important for ensuring their comfort and well-being during this sensitive time. Here are some practical tips for preparing meals:
- Focus on creating small, nutrient-dense meals that are easy to consume. This approach can help manage appetite variations and ensure the intake of essential nutrients.
- When planning meals, consider the patient's preferences and dietary restrictions, and include their favorite foods as much as possible to encourage eating.
- Ensure the patient stays well-hydrated by offering a variety of fluids throughout the day. Depending on their preference and dietary needs, this may include water, juices, and soups.
- Soft and easy-to-eat foods can be particularly beneficial if the patient experiences difficulty swallowing. Options like smoothies, soups, and mashed vegetables can provide both nutrition and hydration.
- Frequent, small meals or snacks throughout the day can be easier to manage than larger, less frequent meals. This can also help maintain energy levels and nutritional intake.
- Collaboration with a dietitian or a healthcare provider can offer guidance tailored to the individual's specific nutritional needs and medical conditions, ensuring the most appropriate diet is followed.
How Hospice Handles Nutritional Needs
Hospice care teams prioritize personalized and compassionate care for those nearing the end of life, which extends to how they handle nutritional needs. Understanding that every individual's situation is unique, they work closely with patients, families, and dietitians to create personalized meal plans that address the physical aspects of nutrition and consider the emotional and psychological comfort that food can provide.
These meal plans are designed to accommodate specific dietary requirements, preferences, and swallowing difficulties, ensuring that the food is not only nutritious but also enjoyable and comforting. Hospice care teams are mindful of their patients' changing needs and diminishing appetites, and they adjust meal plans as needed to ensure that patients maintain as much strength and comfort as possible during their final days.
Nutrition plays a vital role in promoting comfort, dignity, and quality of life. By understanding the nutritional needs near the end of life, caregivers and loved ones can provide the best possible support during this difficult time.
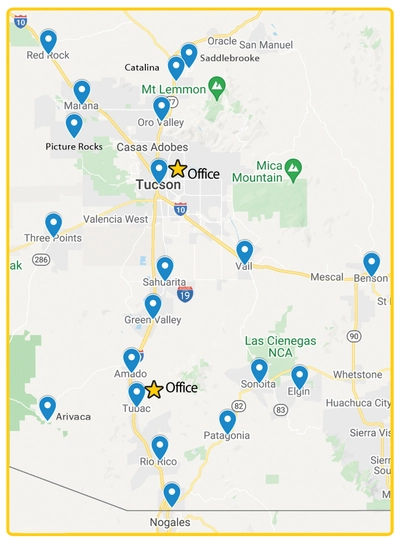
You don't have to navigate this journey alone. Reach out to healthcare providers, palliative care teams, and hospice services for the guidance and support you need. If you’re looking for hospice in Tucson, AZ, contact Soulistic Hospice today. Together, we can ensure that every moment is filled with love, comfort, and the best possible care.